The implementation of the CMS Interoperability mandate has proven challenging for many Health Plans. The rule requires publishing a standards-based Patient Access and Provider Directory APIs, and initiating payer-to-payer data exchange.
Are you facing issues maintaining your API platform? Is your vendor responsive? Is your current vendor sunsetting their support? You may be considering your options, particularly in light of CMS doubling down on HL7 FHIR in their latest proposed rule. Are you ready for the expanding use of FHIR data exchange.
Checklist for Selecting Your Interoperability Partner
Here are 6 factors to consider as you search for the right Interoperability platform:
1. Track Record
When selecting a vendor, consider their track record of successfully delivering interoperability solutions. Are clients satisfied and willing to provide references?
2. Managed Compliance Solution
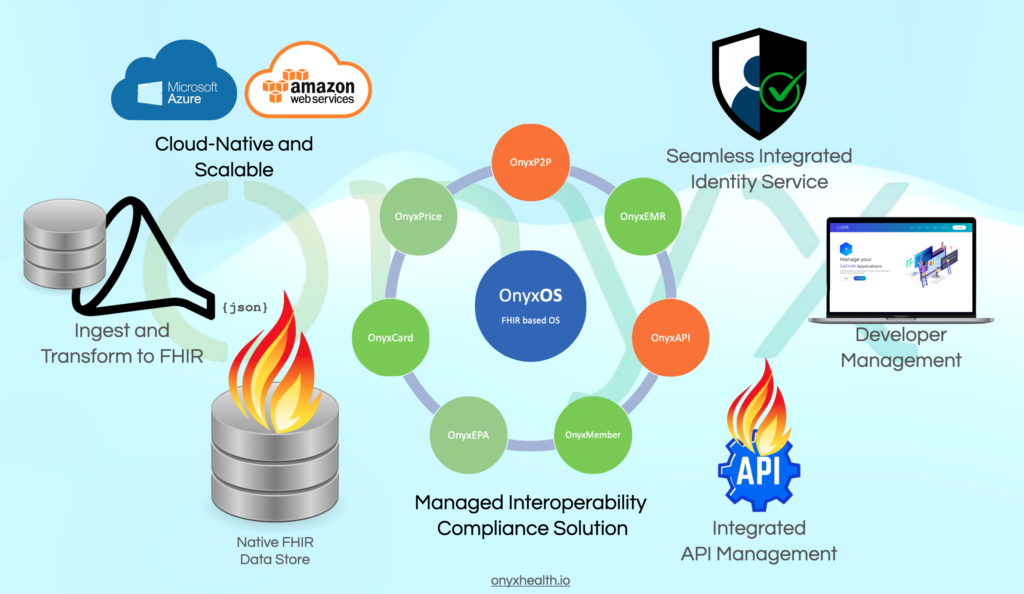
Find a vendor that offers a complete managed compliance service solution rather than a custom-build solution. Since the FHIR specifications are complex and implementation guides continue to evolve, it’s better to consider a comprehensive, end-to-end managed services solution.
3. Expertise
Does the vendor have the necessary competencies to address new rules and regulations? Are they ready for Payer-to-Payer, Electronic Prior Authorization and expanded Patient Access API compliance. Find vendors that are active in workgroups and writing specifications.
4. Cloud Platform
Does the vendor have the active supported of a large cloud platform vendor? For example, Do they offer a co-sell solution that is actively supported by the cloud vendor (such as with Microsoft)? If they do, it indicates a higher level of commitment, than for a one-off implementation.
5. Team
The team assigned to your project is critical to the success of your implementation. Ensure that they have the necessary experience and competence to implement these solutions. Have they successfully taken multiple clients live?
6. Data Extracts
If you are moving to a new platform, it’s crucial to check whether the new vendor can reuse your existing data extracts. This will minimize rework and speed up your transition.
Why Onyx?
Onyx is a vendor that provides a “Managed Interoperability Compliance Solution” for CMS Interoperability and beyond. Onyx’s team built the Blue Button 2.0 API for CMS. We know scale. Which is why our platform currently supports 4% of the US Regulated Plan member population. We don’t just provide a solution, we AUTHOR standards for the industry. We know what it takes to implement successfully. As a result, Onyx has successfully completed many implementations from start to finish within 10-12 weeks. The Onyx platform has won the Frost and Sullivan award for best practices in Interoperability. Onyx is active in industry workgroups. For example, the Payer-to-Payer data exchange guide was authored by Mark Scrimshire, Chief Interoperability Officer of Onyx.
If you’re interested and want to know more, you can contact Onyx at info@onyxhealth.io.
